Greetings from the President
 My name is Dr. Shokichi Teramoto. As the President of the Clinic, I am
responsible for overseeing our treatment policies. Our corporation was founded in 2007, based upon the concept held in common by the late Dr. Osamu Kato, the former Founder and Director of Kato Ladies Clinic, and myself, of “no success, no fee”.
My name is Dr. Shokichi Teramoto. As the President of the Clinic, I am
responsible for overseeing our treatment policies. Our corporation was founded in 2007, based upon the concept held in common by the late Dr. Osamu Kato, the former Founder and Director of Kato Ladies Clinic, and myself, of “no success, no fee”.
However, at the same time, we retained an apparently practical policy in which “infertility treatment means delivering all the possibilities for pregnancy by providing the adequate amount of medication for women who have retained their ovarian functions for them to become pregnant”. In other words, our treatment principles were based on (1) adjustment of the menstrual cycle by using contraceptive pills in order to homogenize the follicular development; (2) suppression of untimely early ovulation by the use of clomiphene; and (3) adequate ovarian stimulation by the use of a follicle stimulation hormone (FSH) drug, and only those who could avail themselves of these treatments were eligible for our contingency pricing scheme.
This was a method in which the higher the level of the ovarian functions, the more results were brought about. On the other hand, for those with reduced ovarian functions, the stress of the treatment increased, and sometimes the reaction to the treatment caused a disturbance in the menstrual cycle, leading to an increase in the FSH level. Around that time, a new test for diagnosing ovarian function by assessing the level of anti-Mullerian hormone (AMH) became available, and it turned out that the lower the level of AMH, the bigger the reaction to the treatment. In fact, it has turned out that as much as 90% of patients had the potential for such a reaction, and 60% would definitely suffer from it. This meant that our conventional treatment had the potential to harm ovarian functions in most of the patients, despite the fact that it was a low-stimulation protocol. As we had thought our low-stimulation protocol was the friendliest treatment for our patients, we were very dismayed when this suspicion became a certainty, and we realized that our treatment aimed at realizing people’s hopes might on the contrary be extinguishing them.
For this reason, we entirely changed our treatment policy three years after the founding of the clinic to one that dispensed with the use of contraceptive pills and ovarian stimulation. Since then, we have completely abandoned all ovary-stimulating drugs, and started a treatment with a “no-stimulation” protocol, which strictly eliminates the use of any stimulation, however low-level it may be.
So we arrived at our present treatment philosophy of “no success, no fee; and no drugs means success”.
IVF at Natural ART Clinic Nihombashi
In order to harvest a good-quality oocyte (egg), one must pay attention to the process of oocyte maturation in the ovary. The maturation process is a very long one: it takes nearly a year for a mature oocyte to develop from the primordial follicle, and the oocyte is profoundly influenced by the pituitary hormones, such as the FSH (follicle-stimulating hormone), in the last few months of the maturation process. This is why we use natural cycle IVF as our fundamental treatment, so that the maturation of the oocyte during the given period is not disturbed. Even when the administration of drugs is necessary, we select the type carefully, use a minimum dose, and make sure not to use hormones which do not naturally exist in the body or the administering of which would exceed the amount naturally tolerated by the body, especially those drugs related to hCG (human chorionic gonadotropin) and FSH. This is because we believe that letting the oocyte grow and be ovulated in the condition closest to nature is extremely important, not only for the “current oocytes,” which are growing now and about to be ovulated, but also for the “future oocytes,” which will be ovulated in the subsequent cycle or later. Here, please let me introduce our unique treatment protocols based on these ideas.
Complete Natural Cycle IVF Treatment
 Touch to open
Touch to open
This is the fundamental treatment protocol of our clinic. Every woman’s oocyte has a different way of arriving at ovulation. Every woman has a distinct idiosyncrasy in the speed of follicular growth, the manner in which the female hormone (estradiol: E2) increases, and the timing at which the oocyte reaches ovulation. The oocytes of those who have had hormone drugs administered in the past might have deviated from natural conditions, and thereby not be able to go through the process of normal ovulation. Natural cycle IVF is important for grasping such “idiosyncrasies” and “the level of deviation”. Ovarian reserve (the capacity of the ovary to provide oocytes capable of fertilization) diminishes as women grow older. This is an unavoidable fact.
However, we believe we must refrain from administering potent drugs, contraceptive pills, and large amounts of ovarian stimulating drugs when the condition of the ovary is poor because they may deteriorate its condition further, endangering its ability to recover naturally. Natural cycle IVF is important for accurately assessing ovarian reserve.
What is more important than anything is the fact that natural cycle IVF is the cycle in which a good-quality oocyte is selected by nature. The dominant follicle selected in natural cycle IVF harbors, regardless of the woman’s age, the best oocyte in the given cycle, and this is what will be waiting for you. However much the ovarian reserve diminishes, the oocyte which will grow into a healthy baby always remains in the ovary.
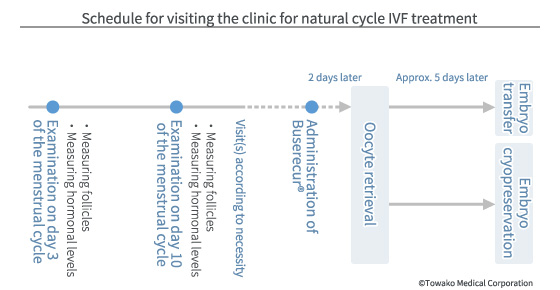
The third day of the menstrual cycle (day 3) is the basic examination day. The basic information, such as the number of follicles (the sac which contains the oocyte; roughly 5mm in diameter on day 3 of the cycle), and the levels of FSH and AMH (the anti-Mullerian hormone which is an index for assessing the number of follicles) are measured. With natural cycle IVF, no drugs are used and the growth of the follicles is closely monitored.
The second visit to the clinic is normally on day 10 of the cycle (those who have had treatment in our clinic and have a record of ovulation occurring before day 10 may be designated to visit either on day 8 or day 9 of the cycle). For some patients, the date for the oocyte retrieval (taking out the eggs) may be decided as early as on the second visit. However, most patients are given the date for the third visit based on the data taken during the second visit.
After a couple of visits, the date for retrieving the oocyte is decided, when the level of female hormone (E2) and the size of the dominant follicle become optimal. Normally, when the E2 level reaches 250 pg/ml, the preparation for oocyte retrieval is set. In the case where the level of brain hormone (luteinizing hormone: LH) has not risen to the optimal level, a nasal spray of GnRH agonist (such as Sprecur® and Buserecur®) is administered to raise the level artificially, and then oocytes are retrieved two days later in the morning (scheduled oocyte retrieval). When the level of LH has risen earlier than expected, secretion of LH may be temporarily suppressed or the action of LH may be offset through the administration of a drug, and then the oocytes are retrieved two days later as planned (suppressed oocyte retrieval). However, if that is not feasible, oocytes are retrieved immediately before the ovulation on the day of the visit or the following day, following the course of nature (emergency retrieval).
When the oocytes have been successfully retrieved and the fertilized embryos have grown into blastocysts that meet the criteria on the fifth day of retrieval, one of these fresh embryos is transferred to the womb without being frozen, as long as there are no problems with the endometrium and the luteal function. However, if the development of the embryos is slow and/or there are problems with the endometrium and/or the luteal function, embryos are frozen, and one of them is thawed and transferred in the subsequent cycle.
* N.B: In our clinic, all patients are provided with oocyte retrieval based on natural cycle IVF protocol which is eligible for the contingency pricing scheme for their initial IVF treatment (on the condition that you can visit the clinic within the designated time frame on the designated days), except for those with amenorrhea and severe cases of menstrual disorder.
Quarter Clomiphene (qC) Cycle IVF Treatment
 Touch to open
The oocytes retrieved just before ovulation has the highest rates of oocyte maturation and retrieval. In fact, the best part of natural cycle IVF protocol and its real significance lies in the fact that we are able to retrieve the naturally selected oocyte just before nature itself releases it. Therefore, in natural cycle IVF treatment, it is crucial to grasp the onset of the LH surge (the time when the LH level begins to rise) appropriately, predict the timing of the ovulation accurately, and then retrieve the oocyte just before the ovulation. However, even daily examination leaves a 24-hour gap which may lead to missing the onset of the LH surge, the level of which changes every hour, sometimes every minute. There is always the situation where “Today is too early, but tomorrow will be too late.” Although this situation requires emergency oocyte retrieval, it might not be the best timing because of the restrictions imposed by office hours. In that case, the rate of retrieval of the oocyte and of its maturation would be lower than those of the scheduled and repressed oocyte retrievals.
Touch to open
The oocytes retrieved just before ovulation has the highest rates of oocyte maturation and retrieval. In fact, the best part of natural cycle IVF protocol and its real significance lies in the fact that we are able to retrieve the naturally selected oocyte just before nature itself releases it. Therefore, in natural cycle IVF treatment, it is crucial to grasp the onset of the LH surge (the time when the LH level begins to rise) appropriately, predict the timing of the ovulation accurately, and then retrieve the oocyte just before the ovulation. However, even daily examination leaves a 24-hour gap which may lead to missing the onset of the LH surge, the level of which changes every hour, sometimes every minute. There is always the situation where “Today is too early, but tomorrow will be too late.” Although this situation requires emergency oocyte retrieval, it might not be the best timing because of the restrictions imposed by office hours. In that case, the rate of retrieval of the oocyte and of its maturation would be lower than those of the scheduled and repressed oocyte retrievals.
Therefore, in ordinary IVF treatment, the onset of the LH surge is suppressed by drugs in order to avoid such a situation (in other words, unscheduled ovulation). There are two kinds of drugs used for that purpose, namely, gonadotropic hormone (FSH and LH)-releasing hormone agonist and antagonist. The representative trade names for such drugs are Sprecur® and Buserecur® for the agonist, and Cetrotide® and Ganirest® for the antagonist. The IVF cycles which use these drugs are called short, long, or antagonist protocols, and they all share the common characteristic that they stop ovulation by potently suppressing the secretion of brain hormone from the pituitary (i.e. FSH and LH) and at the same time stopping the growth of follicles. As a result, in any of these protocols, it becomes necessary to complement a large dose of drugs, namely FSH or hMG (human menopausal gonadotropin), by injection. In addition, hCG (human chorionic gonadotropin) must be administered by injection in order to induce ovulation.
Compared to these protocols (called controlled ovarian stimulation cycles), our clinic has a different method of suppressing the onset of the LH surge ? “the clomiphene cycle IVF”. Clomiphene is an estradiol (E2) antagonist and it counteracts E2 in the hypothalamus, which is situated in the level above the pituitary in the hypothalamic?pituitary?adrenal axis, preventing the promotion of gonadotropic hormone-releasing hormone secretion. As a result, the increase in the LH level which causes ovulation is stopped. The use of clomiphene is different from the conventional protocol in that the action of clomiphene only makes the brain temporarily forget about the commencement of the LH surge and then, with the use of drugs, such as Sprecur®, the brain is easily reminded of the necessity of the LH surge again. In addition, as it does not suppress the secretion of FSH, the follicular growth is maintained, making it unnecessary to administer drugs for enhancing follicular growth (FSH or hMG drugs).
Clomiphene cycle IVF has thus many advantages. However, the maintenance of follicular growth means the generation of small and middle-sized follicles, sometimes causing the problem of “retained follicles”. This is an abnormality where the follicle has already grown large and the E2 level also has already risen at the beginning of the subsequent menstrual cycle. Once this condition develops, it is difficult to put it back to normal.
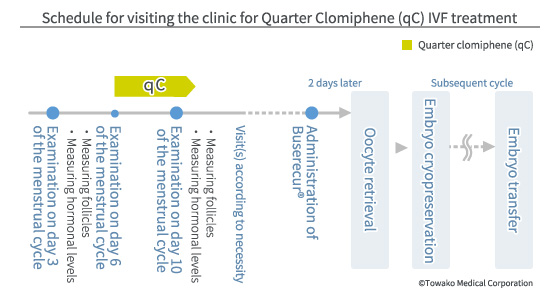
Therefore we have pursued the possibility of drawing only the advantages from clomiphene and devised the method of using a minimal amount of clomiphene for a short period of time ? the protocol called qC cycle IVF. In this protocol, you will take a quarter tablet of clomiphene (12.5mg) daily from day 6 of your menstruation cycle. This low dose (one eighth of the normal dose of 100mg, which you start taking 3 days later than the normal regimen) can effectively suppress the onset of the LH surge and there are hardly any side-effects, and it is as close as one can get to the conditions of the natural cycle.
The schedule for visiting the clinic for examination for qC cycle IVF is the same for natural cycle IVF, but all the oocytes retrieved will be cryopreserved and then thawed/transferred. That is because we take into consideration the effect of clomiphene, even though only a minimal amount is used. With the qC cycle, there will be only one dominant follicle and many small follicles developed, in the same manner as in natural cycle IVF. As there are no middle-sized follicles, all the follicles complete their life-span and normally no remnant follicle remains. Therefore, even if an oocyte fails to be retrieved in the given cycle, it can be retrieved consecutively in the subsequent cycle and the quality of the oocyte will not be degraded.
* Note: The second qC cycle IVF treatment is also eligible for the contingency pricing scheme (on condition that you can visit the clinic within the designated time frame on the designated days, as well as you strictly observe the instructions for taking the drug.)
The Contingency Pricing Scheme
Both the first complete natural cycle IVF and the second qC cycle IVF treatment come under the contingency pricing scheme. With this scheme, the medical fee is restricted to less than 100,000 yen in the case where treatment did not succeed (please see the section on the pricing plan.) The contingency pricing comes into effect when the following conditions are met: consecutive pregnancy for more than 10 weeks has been achieved; the fetal height being more than 30mm, the fetal heart rate being more than 160 times per minute; no apparent abnormality being found with the fetus; and the patient having graduated from our clinic and having moved to a maternity facility for treatment.
letrozole®/Quarter Clomiphene (LqC) Cycle IVF
 Touch to open
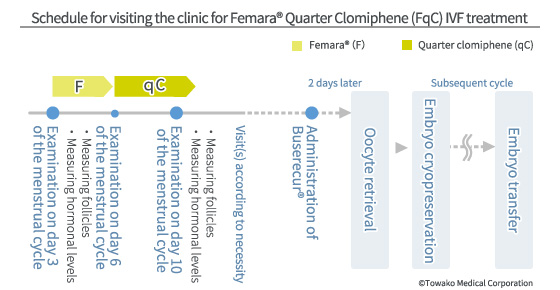
If you could not graduate from our clinic successfully with the treatment by the second trial, letrozole® cycle IVF may be recommended for the third trial and onwards. letrozole® inhibits female hormone generation in follicles (i.e. it is a female hormone synthesis inhibitor). As a result, the hormonal sensitivity of follicles is increased and follicles become able to grow with even a little amount of FSH secretion. Even so, the number of follicles grown is not increased because letrozole® does not have an ovary stimulating effect. This characteristic of letrozole® protocol is almost the same as that for natural cycle IVF. The only difference is the fact that even women with a low FSH secretion level can develop follicles and have ovulation. In particular, the typical candidates for this treatment are women with polycystic ovarian disease (PCO: the only symptom is having a large number of follicles which do not meet the criteria for a pathological condition and the condition is commonly found in Japanese women) and polycystic ovarian syndrome (PCOS: this meets the criteria for a pathological condition and is commonly found in European and American women) whose hormone balance has been disrupted with high LH and low FSH secretion due to too many small follicles.
Touch to open
If you could not graduate from our clinic successfully with the treatment by the second trial, letrozole® cycle IVF may be recommended for the third trial and onwards. letrozole® inhibits female hormone generation in follicles (i.e. it is a female hormone synthesis inhibitor). As a result, the hormonal sensitivity of follicles is increased and follicles become able to grow with even a little amount of FSH secretion. Even so, the number of follicles grown is not increased because letrozole® does not have an ovary stimulating effect. This characteristic of letrozole® protocol is almost the same as that for natural cycle IVF. The only difference is the fact that even women with a low FSH secretion level can develop follicles and have ovulation. In particular, the typical candidates for this treatment are women with polycystic ovarian disease (PCO: the only symptom is having a large number of follicles which do not meet the criteria for a pathological condition and the condition is commonly found in Japanese women) and polycystic ovarian syndrome (PCOS: this meets the criteria for a pathological condition and is commonly found in European and American women) whose hormone balance has been disrupted with high LH and low FSH secretion due to too many small follicles.
One shortcoming of using letrozole® alone is the difficulty of retrieving the oocyte at the best timing because it is hard to predict the shift in the level of the female hormone. In order to conquer this point, we combine the use of letrozole® with the aforesaid qC cycle protocol (thus LqC cycle IVF) in order to prevent the onset of the LH surge and to realize the best timing for oocyte retrieval.
Another disadvantage of letrozole® is the fact that using it for treating infertility is off-label use. letrozole® is marketed as a medicine for treating breast cancer. Because of that, the effects on the fetus have not been studied and therefore the utmost care needs to be taken with regard to its safety. As a precaution, we do not transfer embryos in the cycle letrozole® is administered. The embryo is cryopreserved and transferred in natural cycle IVF protocol in the subsequent cycle or later where there is no influence of letrozole®.
We also pay attention to the dose and the period for administration in order to secure safety: letrozole® is only administered for three days from day 3 of the menstrual cycle. This is because in this way we can make sure that letrozole® will not remain in the body after day 12 of the menstrual cycle because of the drug’s half-life. In other words, the oocytes existing at the time of ovulation will not be influenced by letrozole®. In this LqC cycle also, there are only one dominant follicle and many other small follicles. Therefore, oocyte retrieval can be carried out in the subsequent cycle consecutively, in the same manner as in natural cycle and qC cycle, which promises the harvesting of good-quality oocytes.
The schedule for visiting the clinic is the same as that for natural cycle IVF. Normally, the second visit to the clinic will be on day 10 of the menstrual cycle. When the E2 level has reached 250 pg/ml or more, the day for oocyte retrieval is decided based on your history with natural cycle IVF and qC cycle IVF treatment.
* N.B.: The third LqC cycle IVF treatment is not eligible for the contingency pricing scheme.
Retrieving Oocytes and Sperm
Oocyte (egg) retrieval is carried out by piercing follicles in the ovary with a thin hollow needle put through via the vagina, thereby sucking out the oocyte. As oocyte retrieval is a procedure equivalent to an operation, where the needle penetrates through the abdominal cavity, it is accompanied by the risk of bleeding and infection. Bleeding could be generated by injuring the arteries or veins in the ovary and the surrounding area. We keep bleeding to the ultimate minimum by using a color Doppler ultrasound device and an exclusive extra-thin needle with a specially processed tip. Infection could be caused by bringing a contaminated substance inside the body. We use the original variable suction pressure needle to prevent bringing into the body the follicle flushing liquid or the needle rinsing liquid, thereby managing to keep the risk of infection extremely low. In addition, the clinic’s exclusive needle makes it possible to retrieve oocytes without any form of anesthesia or with minimal local anesthesia. As this imposes less physical stress on the body, patients only have to rest for just 30-40 minutes after the procedure.
As for the sperm, either fresh or frozen/thawed sperm will be used for fertilization. The fresh sperm are retrieved in the semen collection room at the clinic on the day of the oocyte retrieval. The frozen sperm will have been collected and kept frozen, and thawed in advance to be used for fertilization. In the case of azoospermia (a condition of not having a measurable amount of sperm), either percutaneous epididymal sperm aspiration (PESA), where sperm are retrieved from the epididymis by piercing a needle through the skin, or testicular sperm extraction (TESE), where sperm are retrieved from the epididymis surgically, are performed. As sperm retrieved with PESA are suited to be kept frozen, they will have been retrieved and frozen before the day of the oocyte retrieval. On the other hand, as the sperm retrieved with TESE are better used fresh, the oocyte will have been retrieved and kept frozen before the day of the sperm collection. Both methods are our unique procedures and we will provide you with a detailed explanation when you visit our clinic.
Oocyte Retrieval from Small Follicles
 Touch to open
In natural cycle, only one follicle is selected out of the many that exist and this develops into the “dominant follicle.” With younger women with no treatment history, it can be said that the dominant follicle is the one that harbors the best oocyte. However, this natural order begins to be disrupted as the woman becomes older and under the influence of hormonal drugs her menstrual period begins to be disrupted. In fact, there is no rule that there is only one good-quality oocyte that can develop into a baby in a given cycle. For instance, when the dominant follicle exists in the right ovary, you cannot say with certainty that there is no follicle which harbors a good-quality oocyte in the left ovary. It may be that the oocyte in the left ovary is equally of good-quality but it has just not developed. And considering the fact that most of the women who receive IVF treatment are in their late 30s or early 40s and are experiencing the disruption of the menstrual cycle caused by hormonal drugs, it seems obvious that relying only on the dominant follicle in the natural cycle will not give you a good chance of encountering a good-quality oocyte.
Touch to open
In natural cycle, only one follicle is selected out of the many that exist and this develops into the “dominant follicle.” With younger women with no treatment history, it can be said that the dominant follicle is the one that harbors the best oocyte. However, this natural order begins to be disrupted as the woman becomes older and under the influence of hormonal drugs her menstrual period begins to be disrupted. In fact, there is no rule that there is only one good-quality oocyte that can develop into a baby in a given cycle. For instance, when the dominant follicle exists in the right ovary, you cannot say with certainty that there is no follicle which harbors a good-quality oocyte in the left ovary. It may be that the oocyte in the left ovary is equally of good-quality but it has just not developed. And considering the fact that most of the women who receive IVF treatment are in their late 30s or early 40s and are experiencing the disruption of the menstrual cycle caused by hormonal drugs, it seems obvious that relying only on the dominant follicle in the natural cycle will not give you a good chance of encountering a good-quality oocyte.
 Touch to open
However, it is thought that, in the natural cycle, when the dominant follicle has fully developed, all the other non-developed follicles (called small follicles) will be closed and the oocytes inside them will die. Therefore, in common IVF treatment, follicles are potently stimulated with procedures called short, long, or antagonist cycles, in order to develop as many follicles as possible. These approaches seem to make sense on the surface but they require several conditions to be met. For example, there should be many follicles which can respond to the stimulation; these follicles should develop en bloc (in synchronization); and the oocytes in these follicles should be of good quality. In reality, however, one cannot expect women receiving IVF treatment to have these ideal conditions and the success rate per single treatment (live birth rate) is around 10% for a woman who is 38 years old. And, if the initial treatment should fail, what becomes a big problem is whether one can still have the same environment for the second trial when the unexpected drug use (stress) may have wreaked havoc on the body. Each time humans forget to respect nature, they suffer from reprisals, but we still seem unable to apply the lessons we should have learnt. Our clinic’s explanatory meeting session for would-be patients is geared to have you understand this mechanism in detail. Please come and listen to a further, more detailed explanation.
Touch to open
However, it is thought that, in the natural cycle, when the dominant follicle has fully developed, all the other non-developed follicles (called small follicles) will be closed and the oocytes inside them will die. Therefore, in common IVF treatment, follicles are potently stimulated with procedures called short, long, or antagonist cycles, in order to develop as many follicles as possible. These approaches seem to make sense on the surface but they require several conditions to be met. For example, there should be many follicles which can respond to the stimulation; these follicles should develop en bloc (in synchronization); and the oocytes in these follicles should be of good quality. In reality, however, one cannot expect women receiving IVF treatment to have these ideal conditions and the success rate per single treatment (live birth rate) is around 10% for a woman who is 38 years old. And, if the initial treatment should fail, what becomes a big problem is whether one can still have the same environment for the second trial when the unexpected drug use (stress) may have wreaked havoc on the body. Each time humans forget to respect nature, they suffer from reprisals, but we still seem unable to apply the lessons we should have learnt. Our clinic’s explanatory meeting session for would-be patients is geared to have you understand this mechanism in detail. Please come and listen to a further, more detailed explanation.
 Touch to open
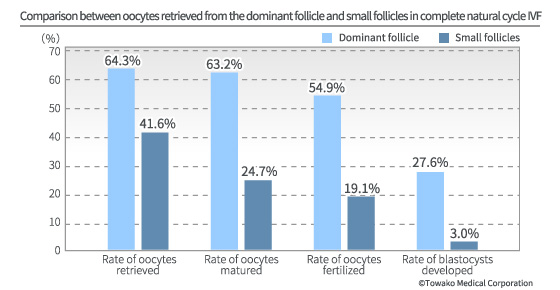
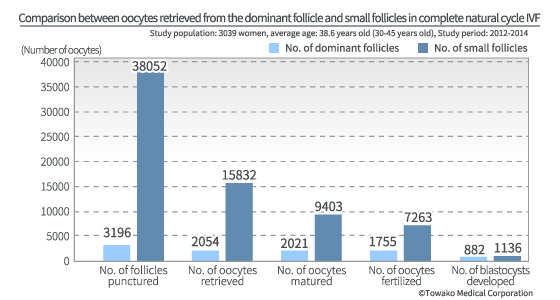
Well, the crucial question is whether or not there is indeed no normal oocyte which can develop into a healthy baby in the follicles which have stayed small as they have not been stimulated by drugs. This question has unfortunately been totally disregarded until now. However, we have taken up this question and have found the evidence for the answer. Only our long experience of earnestly grappling with natural cycle IVF could have allowed us to carry out such an endeavor. As a result, we have found out that there are indeed many normal oocytes in the small follicles which have not been developed as the dominant follicle. And we have become the only IVF center in the world where such small follicles are utilized and which is achieving clinically significant results. There are mature and immature oocytes in the small follicles. Still, many of them infallibly harbor good-quality oocytes, the number of which exceeds that of oocytes derived from the dominant follicle (882 vs 1136).
Touch to open
Well, the crucial question is whether or not there is indeed no normal oocyte which can develop into a healthy baby in the follicles which have stayed small as they have not been stimulated by drugs. This question has unfortunately been totally disregarded until now. However, we have taken up this question and have found the evidence for the answer. Only our long experience of earnestly grappling with natural cycle IVF could have allowed us to carry out such an endeavor. As a result, we have found out that there are indeed many normal oocytes in the small follicles which have not been developed as the dominant follicle. And we have become the only IVF center in the world where such small follicles are utilized and which is achieving clinically significant results. There are mature and immature oocytes in the small follicles. Still, many of them infallibly harbor good-quality oocytes, the number of which exceeds that of oocytes derived from the dominant follicle (882 vs 1136).
The original aspiration needle that supports oocyte retrieval from small follicles
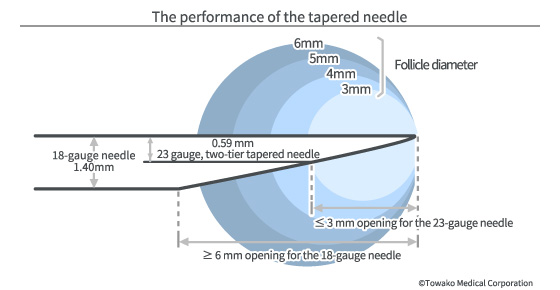
We started developing our clinic’s original aspiration needle in 1999 and now are using the extra-thin needle (23.5 gauge) which is less than half the thickness of the world standard (18-19 gauge.) However, as it is too thin from the point of view of flow velocity and ease of handling, we have developed an original technique called “the two-tier taper” in order to secure the same performance as that delivered by thicker needles.
 Touch to open
Touch to open
The blade at the tip of the needle is processed with a special technology in such a way that it can keep the damage to the tissues to a minimum. With this extra-thin needle, pain and bleeding is also kept to a minimum, making unnecessary the general anesthesia which is routinely given in other fertility centers. It only takes a few minutes normally to finish the oocyte retrieval in our clinic so that you only need to lie down briefly (20-40 minutes) after the procedure and then you can go home during the day. The biggest merit of our original needle is its ability to puncture very small follicles ? as small as 3 mm in diameter. As the size of small follicles is normally 3-6 mm, retrieving oocytes from small follicles is very easy with this needle as long as the physician is skilled at it. This two-tier tapered needle is extremely effective for puncturing small follicles in natural cycle and letrozole® cycle IVF. With our innovative technique to retrieve oocytes from all retrievable follicles regardless of their size, a high pregnancy rate that could not have been imagined in the past has been achieved across all ages from young to elderly.
Please see the scientific literature regarding this technique at the following site of Fertility and Sterility®. URL:http://www.fertstert.org/article/S0015-0282(16)30048-6/fulltext
Male Infertility
Detailed analysis of sperm indicates that many cases of infertility with unknown causes are in fact caused by male infertility. Repeated IVF failures, where it seems a woman cannot get pregnant however many times she has embryo transfer, are in fact often caused by severe cases of male infertility. However, the condition of male infertility is often misunderstood due to blind faith in the WHO criteria. The real problem with male infertility lies in the morphological abnormalities of sperm which cannot be diagnosed with an assessment method such as that adopted by WHO. In fact, many cases of infertility where the cause is thought to be unrelated to male infertility may in fact be caused by severe cases of male infertility.
Sperm abnormality is revealed by analyzing high precision video images and specially stained images using computer technology. Our original devices and internally developed analytical software application make possible an accurate diagnosis of sperm abnormality in a short period of time, thus allowing us to decide on the best insemination method. Furthermore, men with severe cases of male infertility are immediately given hormonal tests and testicle palpation in order to screen for the abnormalities without delay, such as a central defect in spermatogenesis and varicocele, so that treatment for male infertility can be performed simultaneously with ART (Assisted Reproductive Technology) treatment. Good-quality sperm is just as important as good-quality oocytes and it is our clinic’s treatment philosophy to pay equal attention to oocytes and sperm.
Sperm Collection from Epididymis and Testicles
These are procedures for men whose sperm cannot be found in the ejaculated semen. In the case of obstructive azoospermia, sperm are collected from the epididymis with an aspiration needle by piercing through the skin (PESA) and the whole procedure takes only a few minutes. When PESA does not seem to work, biopsy will be performed to retrieve tissues from the testicle and then sperm are extracted from them. This procedure (TESE) takes approximately 30 minutes and is more invasive than PESA. When it is predicted that it would be difficult to retrieve sperm with TESE, sperm must be retrieved under the microscope (MD-TESE). We perform all the above procedures and as long as you have one good-quality sperm, it can be fertilized with the procedure called intracytoplasmic sperm injection (ICSI).
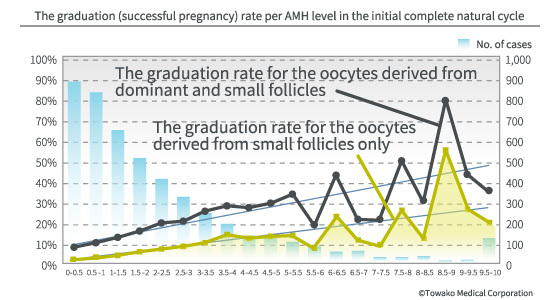
Our thoughts on the aging of oocytes
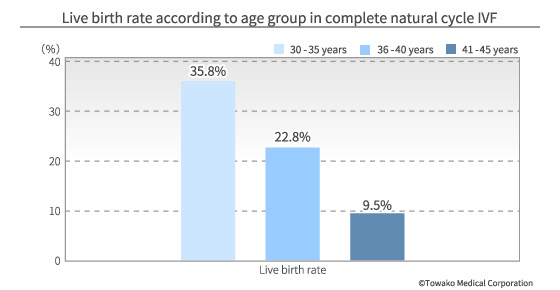
Recently, we often hear about aging oocytes. It is said that the quality of oocytes rapidly goes down as you age, especially after you hit your late 30s. But is this really true? Certainly, the number of primordial follicles and the number of follicles in the cycle with developmental ability decrease as you age. However, that and a decline in quality are different stories. If the quality of oocytes declines after a certain age, the pregnancy rate should also rapidly decline at a certain threshold of the AMH (anti-Mullerian hormone) level. Yet, our data (pregnancy rates based on the oocyte retrieval cycle according to the level of AMH) shows that there is a direct proportional relationship between the pregnancy rate and the AMH level. This means we can expect to achieve pregnancy according to the number of oocytes, regardless of age, and aging does not mean a decline in the quality of oocytes. Because we humans are higher organisms, the rate of our good-quality (normal) oocytes is not that high from the beginning. Therefore, as the number of oocytes decreases, the likelihood of having a good-quality oocyte in the follicle selected as the dominant one will also go down, and the incidence of abnormal chromosomes will go up, too. Furthermore, a decrease in the number of follicles affects the various hormonal controls, leading to a decline in the selectivity of good-quality follicles. Still, these facts are only relevant to the dominant follicle, the selection of which is dealt by natural ovulation, and this is the reason why the live birth rate after the late 30s decreases.
 Touch to open
Touch to open
However, with our IVF method, we retrieve oocytes from all the penetrable oocytes, i.e. not only from the selected dominant follicle but also from the unselected small follicles as well. Therefore, if there is a good-quality oocyte somewhere, we can definitely find it. In other words, retrieving all the follicles, large and small, means replenishing the decreased natural selectivity. The important thing is that these small follicles would never be ovulated naturally and never would be fertilized except by ICSI. These oocytes in the small follicles only come into this world by an artificial procedure, namely oocyte retrieval and embryo culture, and then develop into a baby.
The root of the decline of the pregnancy rate with aging may lie in the decline in the number of the oocytes, rather than a decline in the quality of the oocytes. From this point of view, it can be said that there is a good possibility that you still have good-quality oocytes in your ovary, however few they may be, as long as you have periods with natural ovulation. As you may not be able to encounter such a good-quality oocyte in every cycle, it may take a little while, but if you have a strong will and if you do not do things to prevent you from achieving your aim, you should definitely be able to encounter such an oocyte.
The decline in the number of oocytes means the decline in the level of the hormones in the follicle (inhibin) which are controlling the hormonal balance in the brain. This influence is prominent among older patients whose AMH levels have been reduced. For those patients, even the slightest external interference can disrupt the chain reaction of the follicle development (follicles develop in a group for every cycle, such as the group for this cycle, the next cycle, and the cycle after the next, and so on). Therefore it is very important to refrain as much as possible from the improper use of drugs, especially with older patients who do not have much reserve left.
Drugs which induce or inhibit the development of follicles, such as hCG, hMG, clomiphene, and birth-control pills, disrupt the normal chain reaction of follicle development, affecting the quality and the retrieval rate of the oocyte in the subsequent cycle. Unfortunately, in a normal situation, only one oocyte develops in a natural cycle where no ovarian stimulation drugs are administered. Therefore, this kind of argument may look laughable to those who insist that we need to administer stimulating drugs in order to save, say, the 9 oocytes out of 10 who will meet their deaths in vain otherwise. However, is it not obvious that, if we can retrieve oocytes not only from the one developed follicle (the dominant follicle) but also from the 9 not-developed follicles, it is far better not to administer drugs from the point of view of the subsequent cycles? Based on this idea, we have devised and developed the new techniques ? our original natural cycle and the qC cycle. Our message for those patients, who have been inflicted with the utterly hopeless pronouncement that their oocytes are too old, is not to despair because we can help you with techniques that go beyond stereotypical preconceived ideas.
Insemination and Embryo Culture
Once the oocyte and the sperm are prepared, the next step is insemination. Normally, it is performed by sprinkling the oocyte with a vast number of sperm. However, IVF is not like natural insemination because the female body’s ability to select sperm decreases. In other words, sometimes faulty sperm which would never naturally inseminate an oocyte may do just that. Therefore, for men with high rate of sperm abnormalities, sometimes intracytoplasmic sperm injection (ICSI), which selects the good-quality sperm and inseminates the oocyte artificially, may raise the rate of fertilized embryo development. Although the fertilized embryo is usually cultured in vitro (outside the body) for two days and then transferred to the womb in most of the IVF centers, we will always have them cultured up to the blastocyst stage and then transferred to the womb.
Intracytoplasmic Sperm Injection (ICSI)
This is the technique for men who have a limited ability to inseminate oocytes due to problems with the number and the shape of sperm. A retrieved oocyte is pierced with the injection needle and directly inseminated with a sperm. In cases where a high rate of morphological abnormalities in the sperm is observed, we proactively perform intracytoplasmic morphologically selected sperm injection (IMSI) using a high-power microscope.
Blastocyst Culture
With this technique, the fertilized embryo is cultured for longer than normal, namely for 5-7 days, up to the blastocyst stage, the developmental stage of the embryo just before implantation in the womb. The implantation rate per embryo at the 4-cell embryo stage is far below 20%. On the contrary, the implantation rate of accurately evaluated blastocysts is more than 50%. In order to take advantage of blastocyst culture, highly sophisticated observational ability and control techniques are necessary. In our clinic, an extremely sophisticated information analysis is realized through our original successive image management application (ART diary) and the IC chip indicator. With those technologies combined, physicians and embryologists can share information in real time, and the three parties, including the patients, can mutually evaluate the condition of the embryo and the sperm simultaneously.
Assisted Hatching
This is a procedure to remove the shell surrounding the blastocyst (called the zona pellucida). The rate of embryo implantation depends on the number and the morphology of the trophectoderm (TE: cells that help an embryo attach to the uterus and help form the placenta) which composes the outermost layer of the the blastocyst. Therefore it is extremely important to evaluate the condition of the TE accurately. However, the zona pellucida creates great difficulty in observing the TE. In our clinic, therefore, we proactively perform the procedure of removing the zona pellucida in order to maximize the accuracy of TE evaluation.
Embryo Transfer and Cryopreservation
Embryo transfer is the procedure of returning the fertilized embryo which has been cultured in vitro (outside the body) back into the body in the womb. Normally, it is performed using a thin tube called a catheter, and the embryo is transferred through the vagina under the guidance of the clinic’s original transvaginal ultrasonic device. On rare occasions, it is difficult to put the catheter through from the opening of the womb, particularly in women who have undergone cancer treatment. In such cases, the embryo is transferred through the uterine wall using the technique called the transvaginal-transmyometrial embryo transfer method (Towako method) which was devised by Dr. Osamu Kato (the late former director of Kato Ladies Clinic) and improved by him and Dr. Shokichi Teramoto (the President of Towako Medical Corp. and the General Director of Natural ART Clinic Nihombashi and Shimbashi Yume Clinic). We use either of the two methods depending on the situation and deliver the embryo to the uterine fundus.
Catheter for embryo transfer
We use our original thin, flexible catheter. The normal diameter of a catheter is 6 Fr. (1 Fr = 0.33 mm), whereas we have developed a catheter of 2 Fr. in diameter (less than half of the normal thickness). In addition, the material has been changed from hard Teflon to an extremely soft silicon. Although the operability and the softness are usually incompatible and the catheter is normally required to have a certain rigidity, we have conquered this dilemma by our own method.
Single Embryo Transfer (SET)
Ever since the establishment of our clinic, we have devoted ourselves 100% to single embryo transfer (SET) where only one embryo (fertilized egg) is returned to the body in the womb. This is only made possible with our extremely sophisticated cryopreservation technique where the survival rate of the warmed (thawed) blastocyst is 99%. This is a culmination of a number of low-profile techniques, each of which has been polished to the highest level and then combined with the others with precision.
Treatment of endometrial problems
Problems in the endometrium (the lining of the womb), such as polyps, can hinder the ability of the embryo to implant to the womb. When such a problem is found, the simplest, most effective treatment will be performed before the embryo transfer so that the embryo can implant itself to the womb under better conditions. Testing of endometrial problems can be performed easily and quickly using our original catheter without pain (via ultrasonic hysterography).
Embryo Transfer in the Luteal Hormone Replacement Cycle
The biggest advantage of frozen/thawed embryo transfer is that you can transfer the embryo under the best endometrial conditions. We transfer the embryo into the womb under the optimal conditions for getting pregnant through an accurate evaluation of the best endometrial condition and the hormonal values best suited to embryo implantation.
Transvaginal Ultrasound-guided Embryo Transfer
This is the method conceived by Dr. Teramoto, the General Director of this clinic, inspired by the transvaginal-transmyometrial embryo transfer method (Towako method), and presented at the former Japanese Society of Fertility and Infertility (presently Japan Society for Reproductive Medicine) 18 years ago. This is an extremely accurate and innovative transfer method without any unpleasant preparations, such as filling the bladder.
Vitrification
Vitrification is a technique for the cryopreservation of gametes and embryos. We are proactively performing the cryopreservation of blastocysts in order to maximize the synchrony between the endometrium and the embryo. We have developed our own original vitrification solution and using this has raised the survival rate of frozen embryos after thawing to 99%, far surpassing the world standard.
Regarding the Cryopreservation of Redundant Embryos
We perform cryopreservation in order to improve the rate of implantation. However, we do not provide treatment just in order to increase the number of embryos for cryopreservation. We cryopreserve redundant embryos only when they are generated out of a single oocyte retrieval. We believe the aim of life is preservation of the species, and an embryo in which the traits derived from the female and the male partner are unified should be treated as an individual with a life of its own. Therefore, increasing the number of lives which may not be returned to the maternal body is a deviation from the working of nature and cannot be described as the legitimate use of life science.
 Touch to open
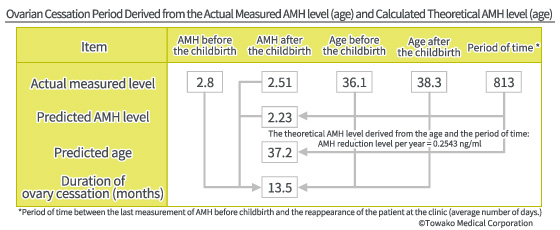
For example, we do not continue oocyte retrieval when there is an embryo (or embryos) to transfer, just for the sake of having a second child. There have been 444 women who had a first child after receiving treatment in our clinic, and then came back again for treatment for a second child within 3 years, since 2011. When their AMH levels were measured and analyzed (which is an indicator for the ovarian function) before and after the pregnancy, the ovarian aging was surprisingly ? or rather we should say expectedly ? suspended for 13.5 months on average. This means it is very likely that the consumption of primordial follicles ceases during pregnancy and after the childbirth until the period is resumed.
Touch to open
For example, we do not continue oocyte retrieval when there is an embryo (or embryos) to transfer, just for the sake of having a second child. There have been 444 women who had a first child after receiving treatment in our clinic, and then came back again for treatment for a second child within 3 years, since 2011. When their AMH levels were measured and analyzed (which is an indicator for the ovarian function) before and after the pregnancy, the ovarian aging was surprisingly ? or rather we should say expectedly ? suspended for 13.5 months on average. This means it is very likely that the consumption of primordial follicles ceases during pregnancy and after the childbirth until the period is resumed.
Indeed, some of the literature has demonstrated that the AMH level becomes extremely low during pregnancy, indicating that the consumption of oocytes is suspended. The reproductive age and individual life-span are the same in many organisms. Perhaps it is the same with humans. As it is thought that the life-span of early humans was around 50 years old at the most, the reproductive age ? the life-span of the ovary ? must have been around that age (late 40s), too. If we presume that women had 5 childbirths or more ? that is had 6 years or longer of ovary cessation periods ? then it is possible that the reproductive age and the life-span of women matched each other, meaning that they must have been able to have babies until their late 40s. From the point of view of the preservation of the species, humans, such as Neanderthals, had to have at least 5 childbirths. Nature perhaps gave various life-spans for each living organism after having worked out everything. In short, if you have a successful childbirth with the first baby, and if you begin the treatment for the second baby approximately 12 months after the delivery of your first one, you hardly need to worry about the degradation of ovarian functions. It is because of this that we insist on focusing on the treatment of the first pregnancy. You do not have to worry about your second baby if you are successful in having the first baby.
Our Treatment Policy
Our mission is to help people suffering from infertility by employing the highest level techniques in the world. It has been 30 some years since the dawn of IVF (in vitro fertilization) and ET (embryo transfer) and since then various techniques have been developed. Especially ICSI (intracytoplasmic sperm injection) and cryopreservation technology have been revolutionary. Yet, their wise use cannot be said to have been established and it seems many problems have been left unaddressed. For example, is it truly the good-quality sperm that is selected in the ICSI? Is the heavy usage of cryopreservation really contributing to the improvement of ART outcomes? Many groundbreaking drugs have been developed and marketed, too. However, the live birth rate for a woman who is 39 years old remains only at 10% (according to the data made public by the Japanese Association of Obstetrics and Gynecology). This fact indicates that the novel technologies do not necessarily bring positive outcomes straight away.
Science deals with nature itself. Not to mention the words of a Nobel laureate, you cannot reach a smidgen of truth unless you embrace the truth without biases. The same is true with the life sciences, which are a branch of science, and the natural cycle is the basis for everything in order to explore the field. Despite this, there is so much interference by artificial stimulations and suppressions in the current situation, and so human nature is masked by a thick layer of drugs. Under such a situation, the development of new drugs does not necessarily mean progress. It is not the same as the progress of natural science, where new intellectual horizons are opened up.
We have firmly maintained a consistent policy of studying the truth of the generation of life through natural cycle IVF and then giving the results back to our patients. In the process, we have been trying to free patients from the use of drugs. This is the fundamental policy of our clinic, a policy initiated by the late Dr. Osamu Kato, inherited by Dr. Shokichi Teramoto, and one we hope will be passed on into the future.
